OT, PT, SLP, and Audiologists working for a school district(s) can refer services in their discipline. In order for Medicaid to accept your referral, you will need to have an NPI, CAQH, and Medicaid number. These numbers are only used for referring and do not keep you from providing or documenting your services. Contact us at info@TeamHBS.com if you have any questions.
Use the links below to apply and revalidate your Referring credentials.
- CAQH (re-attest is required every 3 years in conjunction with Medicaid Revalidations)
- Initially takes about 20-30 minutes to complete
- Re-attest takes about 5 minutes and is only required every 3 years in conjunction with Medicaid revalidations
- 90 re-attests are not required by Medicaid, but may be required by your employer if you work outside of schools.
- CAQH registration directions (Complete CAQH before the Medicaid enrollment.) You will need to enter your CAQH # (CAQH ProView – Self Service Forgot CAQH ID) into the Medicaid application. CAQH info and Tips. CAQH Help Line 1-888-599-1771, Core@CAQH.org CAQH login site
- Medicaid Enrollment & Revalidations
- Initially takes 30-45 minutes.
- Revalidations required every 3 years and can take 5 – 30 minutes depending on work & education changes since previous update
- First time Medicaid applicants: Therapist Medicaid Enrollment Instructions for Referring Providers Medicaid Enrollment assistance & tech support at 1-800-686-1516 option 3, then 3 or email IHD@medicaid.ohio.gov and include your 8-digit OH|ID number
- Therapist Medicaid Revalidation (Detailed) (for therapists already enrolled in Medicaid and are due for their 3 year revalidation)
Q & A
Why do I need these numbers, and why does my service require a referral? The Affordable Care Act (ACA) requires that all services submitted to Medicaid for reimbursement have a referral by a licensed practitioner who is also enrolled in Medicaid to cut down on Medicaid fraud. In order to get approved for a Medicaid number, you must also have your NPI and CAQH number.
Do OTAs and PTAs make referrals or need these numbers? No, OTAs and PTAs are not allowed to make referrals (HB89). Their supervising OT or PT, or another OT or PT connected with that student/district will need to make the referrals.
Will I need to reapply/make updates to my accounts after I obtain my numbers? Yes. Medicaid (PNM) will require that you revalidate/recredential with them (PNM) and CAQH every 3 years. Medicaid/PNM/Maximus will send an email to your “contact email” when this is due. If you have an out-of-state license, you will be required to update it with Medicaid (PNM) each time it’s renewed. Ohio licenses are automatically updated. NPI never requires updates except when initially applying or re-enrolling with Medicaid if previously eligibility lapsed, but you are welcome to update it. *CAQH attestation is only required when initially applying or revalidating your Medicaid number every 3 years. If you don’t work outside of schools, you can ignore the CAQH request to reattest every 120 days.
Do I have to obtain a Medicaid number to document services? No, the Medicaid number (and NPI/CAQH) is only required if you will make referrals. We won’t process any service that is either missing a referral or has a referral from a provider without an active Medicaid number. You can document all of your services without an NPI, CAQH, and Medicaid number. If you are subbing, your services will probably be covered by the primary therapist’s referral or a supervising therapist. If not covered, have another therapist in your discipline who is associated with the student/district make the annual referral for you.
I applied for my Medicaid number. Can I start making referrals even though I haven’t been approved for a Medicaid number yet? Yes, you can add referrals anytime. Medicaid will make your number retroactive up to one year if you selected the “provisional” option that was in our directions. We will hold all services you refer until you are approved for a Medicaid number and we have that number on file. Verify your number is on file here.
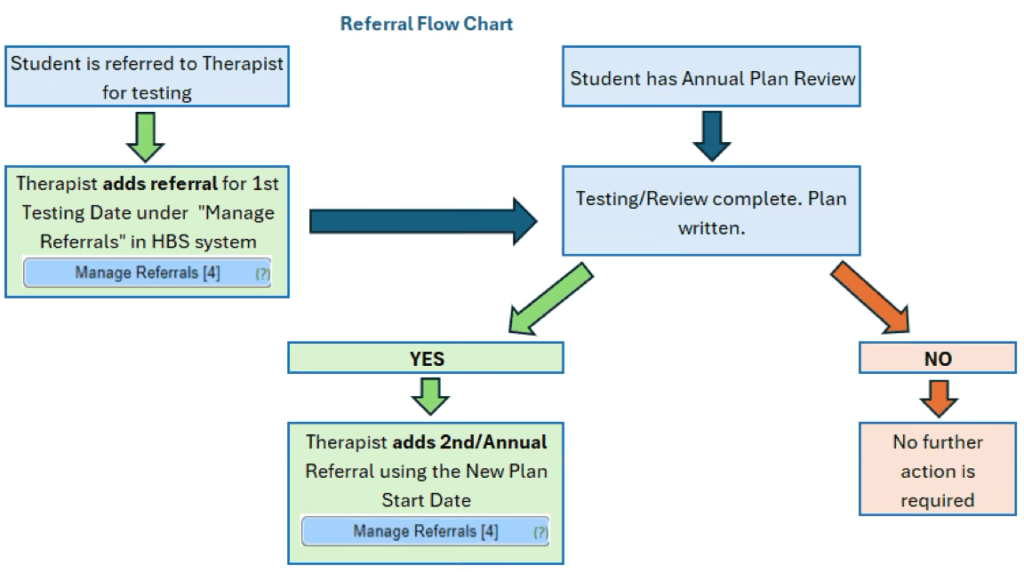
When do I make referrals? 1st Referral is for the initial date of ETR Testing (even if the student doesn’t qualify for an IEP), then the 2nd and Annual Referrals are the IEP Start Date each year the student qualifies. If a student moves into your district or you accept their plan of care, you can make a referral for the date you accept their plan of care.
What is NPI? NPI is your National Provider Number. This number is required in addition to your State Medicaid number in order to make referrals.
What is CAQH? CAQH is a “holder” of provider data. Medicaid subscribes to CAQH, a separate entity, to help with their credentialing requirements.
What is Medicaid enrollment? Medicaid enrollment is required for OT, PT, SLP, and Audiologists to make referrals for services and evaluations.
What is PNM? The Provider Network Management (PNM) system is Medicaid’s enrollment portal. You will login through your OH|ID account and pull up the PNM app to apply, make updates like license expiration dates and name changes, and revalidate through Medicaid’s PNM system.