The Medicaid Eligibility Rate (MER) data for the 2015/16 school year must be submitted to the Ohio Department of Medicaid by March 31, 2016. Billing vendors collect this EMIS information directly from the district, or from their Information Technology Center (ITC), and submit one mass file to ODM. The data submitted contains Student Name, DOB, Zip Code, and IEP Status, as of the 2nd week in October, and is used to compute each district’s IEP Medicaid Eligibility Rate (MER) percentage. This is the only Cost Report factor that is district specific, and its accuracy is critical to maximizing MSP reimbursement.
The standard MER calculation is “Total IEP Medicaid Students” divided by “Total IEP Students”
Example: 48 IEP Medicaid Students divided by 100 Total IEP Students = 48% IEP MER.
Beginning with the 2014/15 school year Cost Report, the MER calculation has changed, and districts will now be penalized for not having a paid claim for all IEP Medicaid students. This is what I have been calling the “Interim Claiming Cost Adjustment”, and is why I have been stressing to districts to obtain a signed Parental Consent Form for all IEP students and make certain that Related Service Therapists are documenting for all MSP billable IEP services.
The new MER calculation will be “Total Number of IEP Students with a Paid Claim” divided by “Total Number of IEP Students with an MSP Billable Service.
Example: 75 Students with an MSP Paid Claim divided by 150 IEP Students with a Billable Service = 50% MER.
Here is an example of the new Cost Report IEP MER calculation. Keep in mind that not all IEP students receive “Billable MSP Services” (green section below), so those students need to be factored out of the equation (denominator).
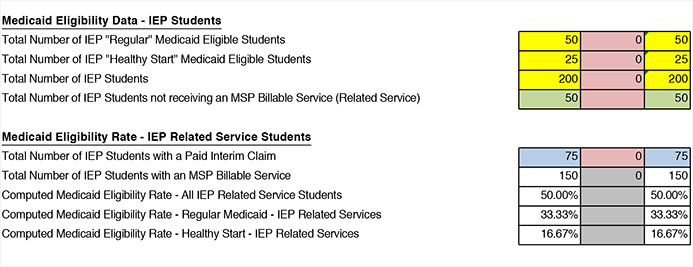
*Note that the column in red is for AUP audit adjustments. When an auditor disallows a claim in the AUP audit, the “Number of IEP Students with a Paid Interim Claim” will be reduced by one, therefore additionally reducing the district MER.
We are getting ready to start the preparation of the 2014/15 MSP Cost Reports, and we need to get a list from each district that shows, as of the second week in October 2014, the IEP students that were receiving a Related Service, and a second list that shows the IEP Related Service students that were receiving “Consult Only” services. To maximize your MER percentage, we want our denominator to show only those students that received an MSP Billable Service. IEP Students that do not receive a Related Service or had “Consult Only”, would have no possibility of having an MSP Billable Claim, and therefore should not negatively affect the district IEP MER.
Not only are we going to use this new data to compute MER percentages, but we are also going to mark the students in our system as a “Related Service Student”, and make sure that there are claims for all related service students. This new methodology has the potential to reduce district’s overall MSP reimbursement, but at the same time, if tracked properly, it could actually increase overall Medicaid reimbursement. Three key components are:
- Provide an accurate list of IEP Related Service Students.
- Make sure that you are obtaining signed Parental Consent forms for all IEP students.
- Make sure that therapists are documenting for All Students.
Most of your IEP software programs should be able to accumulate this new information. IEP Anywhere has an “IEP Related Services Report” that should be able to provide this data. I would suggest accumulating the information for the 14/15 school year (October 2014), and the 15/16 school year (October 2015) at the same time.
It is extremely important that your district and your billing vendor understand this new methodology, and is working towards getting your “Total Number of IEP Students with a Paid Interim Claim” as high as possible. There are still several more months that districts could file Interim Claims for the 2014/15 school year (365 day filing limit). Claims can still be submitted for March, April, May, and June of 2015, but after that, your “Total Number of Students with a Paid Interim Claim” is final.
